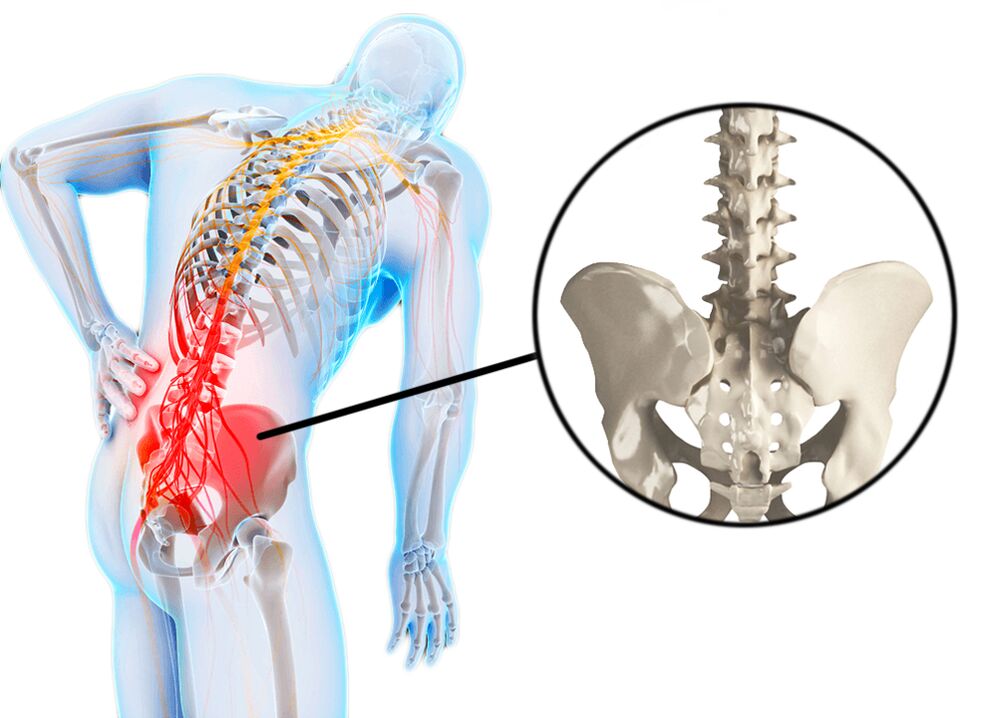
Low back pain is often referred to as low back pain or low back pain. Low back pain or "low back pain" is an acute low back pain, often associated with hypothermia and exertion. Low back pain occurs in many people and is often the cause of temporary disability. Usually, a sports injury or sprain can be the cause of low back pain, but sometimes what triggers the pain is unknown. Low back pain is characterized by pain that does not radiate down the leg. Low back pain (low back pain) can be acute and progress gradually over the course of the day. There is usually morning stiffness and gradually the stiffness turns into a pain syndrome. Curvature of the spine (jet scoliosis) can also be caused by muscle spasms. The pain itself can be caused by muscle spasms, which in turn are related to other causes. This could be an overload or sprain, a sports injury, herniated disc, spondylolisthesis (spondylolisthesis), kidney disease (infection or kidney stones). Patients sometimes pinpoint a cause-and-effect relationship for the occurrence of exertional discomfort and hypothermia, but pain often appears for no apparent reason. Sometimes, back pain can appear even after sneezing, bending over, or putting on shoes. This can be facilitated by deforming diseases of the spine, such as scoliosis.
Unlike low back pain, the term low back pain does not mean acute pain, but subacute or chronic pain. As a rule, pain with paralysis appears gradually over several days. The pain may also occur in the morning and may decrease with physical activity. Paralysis is characterized by pain that increases with prolonged static load (sitting, uncomfortable body position). The characteristic of muscle paralysis is that the pain is relieved when lying in a certain position. Patients with muscle paralysis have difficulty performing daily activities such as washing or wearing shoes due to muscle spasms. Due to the disease, there is a decrease in the volume of movement of the trunk (forward leaning or, to a lesser extent, side tilt or extension). Because of the pain syndrome, patients often have to change positions when they need to sit or stand. Unlike low back pain, muscle spasms are less pronounced and, as a rule, do not cover the entire lower back and are more commonly present with spasms on one side.
Causes of back pain
Back pain is a symptom. The most common causes of back pain are diseases (injuries) of the muscles, bones, and discs. Sometimesback-achecan be caused by diseases of the abdominal cavity, small pelvis and thoracic cavity. Such pains are called reflected pains. Abdominal diseases (eg, appendicitis), aortic aneurysm, kidney disease (urolithiasis, kidney infection, bladder infection), infection of pelvic organs, ovaries - all of thesecan all manifest.back-ache. . . Even a normal pregnancy can lead to low back pain due to sprains in the pelvic area, muscle spasms due to stress, and nerve irritation.
Oftenback-acheassociated with the following diseases:
- Nerve root compression, causes symptoms of sciatica and is often due to a herniated disc. As a rule, when the nerve root is compressed, pain is acute, there is irradiation and decreased sensitivity in the inner region of the nerve root. Disc herniation occurs mainly due to disc degeneration. There is bulging of the glue portion of the disc from the central cavity and pressure on the nerve roots. Degeneration in the intervertebral discs begins at age 30 and older. But the presence of a hernia does not always lead to structural damage.
- Osteoarthritis - degenerative changes occur in the vertebrae themselves, bone growth (osteoporosis) occurs, which can affect neighboring nerves, leading to pain.
- Spinal stenosis can occur due to degenerative changes in the spine (spondylolisthesis and osteonecrosis). Patients with lumbar spinal stenosis may have low back pain that radiates to both legs. Low back pain may occur when standing or walking.
- Cauda equina syndrome. This is a medical emergency. Cauda equina syndrome occurs due to compression of the cauda equina elements (the end of the spinal cord). Patients with equina cauda syndrome may experience pain and impaired bowel and bladder function (incontinence and incontinence). This syndrome requires urgent surgery.
- Pain syndromes such as myalgia or fibromyalgia. Myofascial pain syndrome is characterized by pain and tenderness at certain points (trigger points), reduced volume of muscle movement in painful areas. Pain syndrome is relieved by relaxing the muscles located in the painful areas. With fibromyalgia, aches and pains all over the body. Fibromyalgia is not characterized by tightness and muscle pain.
- Infection of the bones (osteomyelitis) of the spine is rarely the cause.
- Noninfectious inflammatory diseases of the spine (ankylosing spondylitis) can cause stiffness and pain in the spine (including the lower back), which is especially worse in the morning.
- Tumors, often metastatic cancer, can be a source of lower back discomfort.
- Inflammation of the nerves and, therefore, manifestations of pain (in the chest or in the lumbar region) possibly due to damage to the nerves (eg, with shingles)
- Because of the many causes of symptoms, such as acute or subacute low back pain, it is very important to fully evaluate the patient and perform all necessary diagnostic procedures.
Symptom
Pain in the side of the hip is the main symptom of low back pain, hemiplegia, and migraine.
- The pain may radiate to the front, side, or back of the leg (low back pain), or it may be localized to the lower back (lumbar pain, muscle paralysis).
- The sensation of lower back pain may increase after exertion.
- Sometimes the pain can get worse at night or during prolonged sitting, such as during a long car trip.
- Perhaps the presence of numbness and weakness in the part of the leg, located in the inner area of the compressed nerve.
For timely diagnosis and treatment, some criteria (symptoms) need special attention:
- History of recent trauma, such as falls from a height, traffic accidents or similar incidents.
- Presence of minor trauma in patients over 50 years of age (eg, falls from a low height due to slippage and buttock landing).
- History of long-term steroid use (eg, these are patients with bronchial asthma or rheumatic diseases).
- Any patient with osteoporosis (mostly elderly women).
- Any patient over 70 years old: at this age there is a high risk of cancer, infection and diseases of the abdominal organs, which can cause low back pain.
- History of oncology
- Presence of infectious diseases in the recent past
- Temperatures above 100F (37. 7 C)
- Drug use: Drug use increases the risk of infectious diseases.
- Lower back pain aggravated at rest: as a rule, the nature of this pain is associated with cancer or infection, and such pain can also be caused by ankylosing spondylitis (ankylosing spondylitis). joint).
- Significant weight loss (for no apparent reason).
- The presence of any acute nerve dysfunction is a signal for urgent medical attention. For example, this is a violation of walking, dysfunction of the feet, as a rule, are symptoms of acute nerve injury or compression. In certain cases, such symptoms may require an emergency neurosurgery.
- Bowel or bladder dysfunction (both urinary incontinence and urinary retention) can be a sign of a medical emergency.
- If no treatment is recommended or the pain increases, medical attention may also be sought.
The presence of any of the above factors (symptoms) is a signal to seek medical help within 24 hours.
Diagnose
Medical history is important for an accurate diagnosis, as different conditions can cause lower back pain. Time of onset of pain, relationship to exertion, presence of other symptoms such as cough, elevated temperature, bladder or bowel dysfunction, convulsions, etc. v. A physical examination is performed: the identification of pain points, the presence of muscle spasms, a study of the neurological condition is carried out. If disease of the abdominal cavity or pelvic organs is suspected, conduct an examination (ultra-abdominal ultrasound, ultrasound of the pelvic and pelvic organs, blood tests in the urine).
If the etiology of lower back pain is excluded, instrumental investigations such as X-ray, CT, or MRI may be indicated.
X-rays are the initial examination and allow you to determine the presence of changes in bone tissue and indirect signs of changes in the disc.
CT allows you to visualize the presence of various changes, both in bone tissue and in soft stones (especially with contrast media).
MRI is the most informative research method that allows the diagnosis of morphological changes in various tissues.
Densitometry is necessary when osteoporosis is suspected (usually in women over 50 years of age).
EMG (ENMG) is used to identify conduction disturbances along nerve fibers.
Laboratory tests are prescribed (blood tests, urinalysis, blood biochemistry) mainly to exclude inflammatory processes in the body.
Pain treatment
Once the diagnosis and confirmation of vertebral origin with low back pain and paralysis is established, a certain treatment for lower back pain is prescribed.
In acute pain, it is necessary to rest for 1-2 days. Bed rest can relieve muscle tension and spasms. In most cases, when the pain syndrome is caused by muscle spasms, the pain syndrome subsides within a few days without medication, only with rest.
Medicine. For pain syndrome, drugs of the NSAID group are used. COX-2 inhibitors have fewer side effects, but long-term use of these drugs also carries certain risks. Because all drugs in this class have many side effects, they should be taken for a short period of time and under the mandatory supervision of a physician.
Muscle relaxants may be used to reduce spasms. But the use of these drugs is only effective when there is a contraction.
Steroid medications can be used to treat pain, especially when there are signs of sciatica. But due to the presence of pronounced side effects, steroid use should be selective and of short duration.
Manual therapy. This technique can be very effective when there is muscle mass or proliferation of facet joints. Moving the range of motion can relieve both muscle spasms and lower back pain.
Physical therapy. There are many modern physiotherapeutic procedures that can both reduce pain, reduce inflammation, and improve microcirculation (e. g. , electrophoresis, cryotherapy, laser therapy, etc. ).
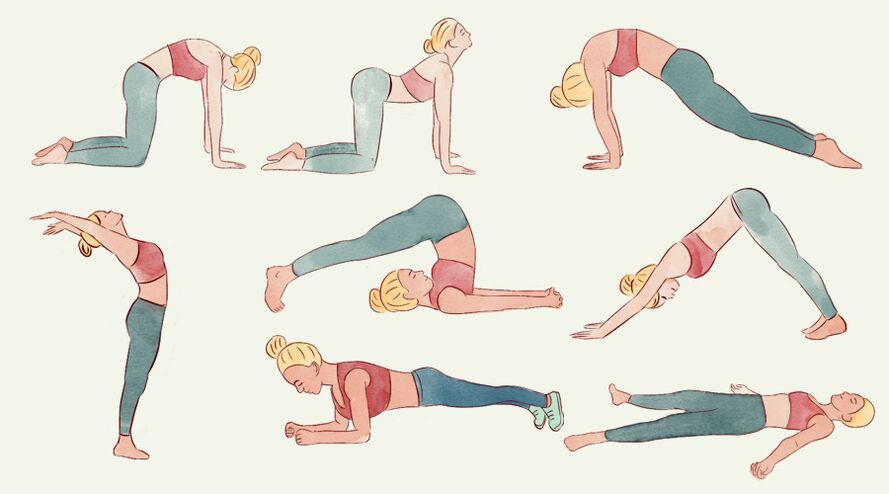
Exercise therapy. Exercise is not recommended for acute low back pain. Linking exercise therapy may be possible after pain syndrome relief. When it comes to chronic pain, exercise can be very effective in increasing muscle strength and improving the biomechanics of the spine. Exercises should only be selected in the presence of an exercise therapist, as stand-alone exercises can often increase symptoms of pain. Systemic exercise therapy, especially when there are degenerative changes in the spine (osteonecrosis, spondylosis), can preserve spinal function and significantly reduce the risk ofpain.

















































